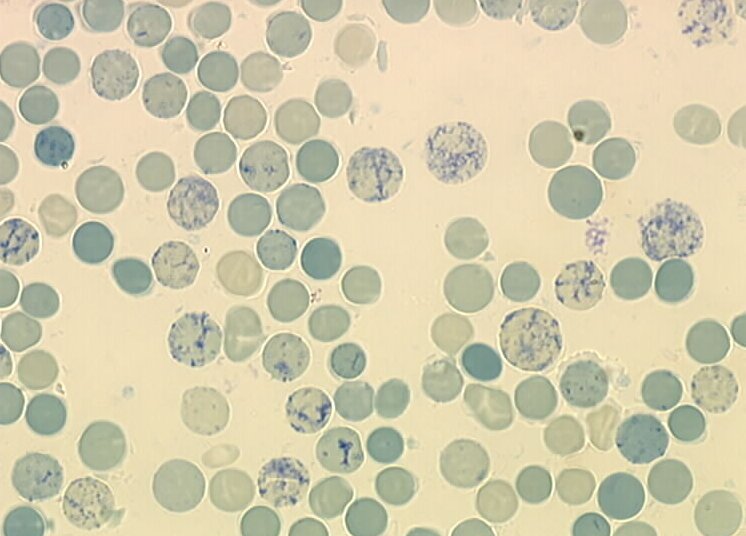
Reticulocytes
What are Reticulocytes?
Reticulocytes are red blood cells that are not yet mature. These immature red blood cells are made in the bone marrow then released into the bloodstream. They circulate in the bloodstream and take two days to become mature red blood cells. Red blood cells are crucial in the transportation of oxygen in the body as they contain haemoglobin a compound that readily combines with oxygen before the cells release it to the entire body.
What is Reticulocyte Count?
Reticulocytes usually make up one percent of all red blood cells in the bloodstream at any one time. Reticulocyte count is performed to find out how the number/percentage immature red blood cells compared to the mature ones. in the bloodstream. This can be used to determine the rate at which the bone marrow produces reticulocytes.
Reticulocyte count used to be carried out by manually by using a microscope to inspect a slide that was specially stained then counting the number of reticulocytes in the field of view. This method had been replaced by the more accurate automated method where an instrument called a hematology analyzer is used.1
Necessity for Reticulocyte Count
- If abnormal results for a complete blood count or hematocrit are obtained, then a reticulocyte count may be ordered to determine the cause
- Doctors usually order a reticulocyte count for patients to diagnose anemia. The count helps determine if anemia is caused by inadequate production of reticulocytes or loss of mature red blood cells.
- Reticulocyte tests can also be used to monitor effectiveness of treatment for various conditions e.g. anemia.
- Reticulocyte counts are also helpful in diagnosing bone marrow disorders or monitor the effectiveness of a bone marrow transplant.2,3
Preparation
No preparation is needed for a reticulocyte count though it is advised to wear a short sleeved shirt to allow medical professionals easy access when drawing blood. The doctor may however ask you to fast or stop taking certain medications e.g. blood thinners for a certain period before the test.1
Drawing of Blood
- A medical professional wraps a tourniquet (elastic band) on the upper arm stopping the flow of blood. The tourniquet applies pressure causing the veins below the band to swell up with blood so it easier to insert a needle.
- A vein usually on the back of the hand or on the inner side of the arm near the elbow is chosen.
- They then clean a section of the skin around the intended site of puncture using antiseptic or alcohol to kill any pathogens around.
- Blood is then drawn from the vein by inserting a butterfly needle and draining blood into a syringe or vial.
- Once drawing of blood is complete the tourniquet is removed.
- As the needle is removed a cotton ball or gauze pad is placed over the puncture site.
- Pressure is applied to the cotton or gauze to speed up the clotting of blood.
For younger children and infants, the doctor may opt to make a small cut on the skin instead of using a needle. A blood sample is collected using a slide or test slip after the cut begins to bleed. The area is then cleaned and bandaged if necessary.1,2,4
How it Feels?
Drawing blood for the reticulocyte count is a relatively painless experience. There is temporary discomfort that feels like a pinprick or sting when the needle is being inserted. Drawing blood only takes a few minutes and does not cause pain. The puncture site might have mild bruising that clears away in a few days depending on the person’s sensitivity.
Risks Involved
Collecting a blood sample for a reticulocyte count is not a dangerous procedure but some complications may arise
- Difficulty locating a vein may cause pain due to many punctures made in attempts.
- Some people suffer a feeling of faintness or lightheadedness.
- Formation of a hematoma (blood accumulating under the skin) that causes a bruise or lump.
- Phlebitis occurs in a few cases. This is the swelling of the vein after drawing of a blood sample.
- Continuous bleeding may affect people with blood clotting problems or those taking blood thinners like Warfarin or Aspirin.
- An infection may develop at the puncture site.
Meaning of Test Results
Normal
Reticulocyte count is expressed as a percentage of the number of reticulocytes compared to the mature red blood cells. Range of results varies from lab to lab but approximately normal results show that: infants have a normal range of between 3% to 6% whiles adults’ range is between 0.5% – 1.5%.2,5
High
A high count indicates that the bone marrow is producing an unusually large number of reticulocytes.
Conditions of High Reticulocyte Count
- Diseases that cause premature haemolysis (destruction) of red blood cells e.g. hemolytic anemia.
- Excessive loss of blood.
- High altitude raises reticulocyte count to help the body cope with lower oxygen concentration high above sea level.
- Presence of a tumor causing excess erythropoietin
- Polycythemia vera
Low (Below Normal)
Low count indicates that an insufficient number of reticulocytes are being produced by the bone marrow.
Conditions of Low Reticulocyte Count
Reticulocyte count falls below normal under the following conditions:
- Deficiency of folic acid, Vitamin B-12 or iron.
- Some types of anemia e.g. pernicious anemia, iron deficiency anemia or aplastic anemia.
- Exposure to harmful levels radiation either through therapy or as a occupational hazard.
- Damage of the bone marrow by some types of medicine or long term infection.
- Chronic or long term alcoholism.
- Chronic or advanced kidney disease.
- Endocrine disease.
What Can Affect Test Results?
- A blood transfusion that was carried out less than three months before the reticulocyte count can affect the results. One should inform the doctor if they have had a recent blood transfusion.
- Some medicine and treatment options for some illnesses e.g. malaria, Parkinson’s disease, chemotherapy and rheumatoid arthritis affect the reticulocyte count.
- Pregnancy also affects the reticulocyte count.2,3
Interpretation of Test Results
Other tests can be used to supplement a reticulocyte count when further evaluation of a conditionis required; these include:
- Reticulocyte index
- Reticulocyte production index
- Immature reticulocyte fraction (reticulocyte maturity index)
- Bone marrow aspiration and biopsy
Reticulocyte count gives clues as to the disease affecting a patient but does not directly diagnose any particular condition. It requires further tests before a final diagnosis can be made, such tests may include:
- Haptoglobin
- Erythropoietin
- Iron Studies 3,4,5
References
- Blood Test: Reticulocyte Count. Kid’s Health – http://kidshealth.org/en/parents/reticulocyte.html?WT.ac
- Reticulocyte Count. WebMD – http://webmd.com/a-to-z-guides/reticulocyte-count
- Reticulocytes. Lab Tests Online – https://labtestsonline.org/understanding/analytes/reticulocyte/tab/test/
- Reticulocyte Count: Purpose, Procedure, and Results. Healthline – http://healthline.com/health/reticulocyte-count
- Reticulocyte Count and Reticulocyte Haemoglobin Content. Medscape – http://emedicine.medscape.com/article/2086146-overview
